General
1. On approaching a child:
- Look around room: Any medications / nutritional drink lying on the table
- View from Distance
- Nutritional status: ‘ I would like to plot his height and weight on a growth chart’
- ? Failure to thrive
- Well/ unwell: conscious level (hepatic coma)
2. Dysmorphic features (mucopolysaccharidoses)
3. Skin – Colour (sallow / yellow / green / brown)
– Increased body hair / facial hair (ciclosporin)
– Skin rashes: Dermatitis herpetiformis , Telangiectasia (Osler – Weber – Rendu)
– Perioral freckling (Peutz-Jeghers)
– Pigmentation: Café-au-lait spots (Neurofibromataosis 1 – GI stromal tumours –palpable abdominal mass), Incontinentia pigmentosa
4. Nutritional support
- Nasogastric tube
- Total parenteral nutrition
- PEG tube
5. Peritoneal dialysis catheter
6. Urinary catheter – spina bifida
7. Older child in nappies – incontinent (neuro/ behavioural)
Hands:
Finger clubbing (Cystic fibrosis, liver disease, Inflammatory bowel disease, coeliac disease)
Koilonychia (Iron deficiency anaemia)
Leuconychia (Cirrhosis)
Palms:
Palmar erythema (chronic liver disease)
Pallor of palmar crease
Hepatic flat (Liver failure, renal failure, CO2 retention)
Arms
Tuberous (elbow) / tendon xanthomas (hypercholesterolaemia)
Bruising (Liver dysfunction, haematological disorders)
Scratch marks
Spider naevi
Face
Eyes: Jaundice (Sclera), anaemia (Conjunctiva), Kayser- Fleischer Ring
Face plethora: Chronic liver disease
Cyanosis: Hepatopulmonary syndrome -à Transplantation
Mouth: Pigmentation (Peutz- Jeghers syndrome)
Ulcers (Apthous ulcers: Crohn’s disease, ulcerative colitis, coeliac disease, behcet’s disease)
Gum hypertrophy (myeloid leukaemia, ciclosporin, phenytoin)
Tongue: Macroglossia (hypothyroidism, Beckwidth-Wiedemann, mucopolysaccaridoses, Pomps’s GSD, Amyloid, haemangioma, lymphagioma)
Glossitis : Iron, folate, B12 deficiency
Neck and Chest
Spider naevi
Gynaecomastia (chronic liver disease)
Abdomen
- Inspection:
1. Shape
2. ? Distension (central flank?, generalised/ localised, symmetrical?)
– 5Fs : Faeces (Hirschsprung constipation), flatus, fat, fluid (ascities, nephrotic syndrome), fetus
3. Obvious masses
4. Scars: Renal angle scars / Laparoscopic surgery / Liver Biopsy
Groins – inguinal hernia repair, renal transplant (will also be palpable mass)
Below right subcostal margin – (Kocher’s incision) – think cholecystectomy, especially in sickle cell disease, any liver procedure, e.g. hemi-hepatectomy for hepatoblastoma
‘Rooftop scar’ – liver transplant
Transverse upper abdominal incision – repair of congenital diaphragmatic hernia – more common on the left
Upper abdominal midline incision – Nissen’s fundoplication
Small right upper transverse incision – Ramstedt’s pyloromyotomy
Umbilicus – consider gastroschisis or exomphalos, umbilical hernia repair
Laparoscopy scars – more common, very small and multiple (often one at umbilicus)
Lateral thoracolumbar incision – nephrectomy
5. Striae
6. Caput medusae (Blood flows away from umbilicus)
- Differentiate from superior vena cava obstruction (flows inferiorly)/ Inferior vena cava obstruction (flows superiorly)
7. Other: Stomas: Ileostomy vs Colostomy ;
Mucous fistula
Caecostomy tube for entergrade enemas in children with chronic constipation (MACE procedure – Malone antegrade colonic enema)
Mitrofanoff, Peritoneal dialysis catheter
8. Get patient to blow tummy up / flatten tummy
9. Get patient to raise head : hernia / Divarification of recti
- Palpation
- Patient should be on a supine position. However, if patient has gross ascites, you might want to ask him whether it is comfortable for him to lie flat as he might have difficulty breathing if lying flat.
- Be sensitive. Tell the child: ‘ I am going to feel your tummy. Please let me know if you feel any pain or if you want me to stop, ok? ’. Whist palpating, look at the child’s face. If the child’s winced, stop and apologise and ask the child if he is ok.
- If you are tall or the bed position is low, you might want to kneel down when doing palpation.
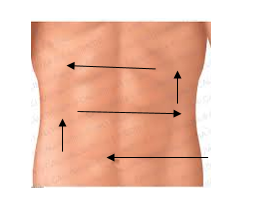
1. Superficial palpation
Palpate systematically. You may start from left iliac fossa and proceed in the direction above.
2. Deep palpation (palpate deeper for deeper masses. Again, warn the child that you are going to feel deeper and ask him to tell you if he feels any pain.
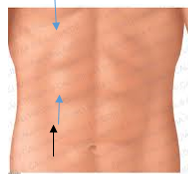
3. Liver (Palpation + Percussion)
Palpate upwards from right iliac fossa towards right subcostal margin until you feel the liver edge. Ask the patient to take a deep breath and try to feel the liver edge as it descends.
If you feel a mass, describe the surface (smooth or nodular) , consistency (hard/ soft) , edge (regular/ irregular)
Percuss from right lower quadrant of the abdomen upwards until the sound changes from resonant to dull. This denotes the liver’s lower border.
Then percuss from right upper chest downwards, starting in the midclavicular line at about the 3rd intercostal space. Percuss inferiorly until dullness denotes the liver’s upper border. Measure the liver span in centimetres
4. Spleen
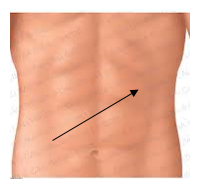
Palpate from right iliac fossa towards left subcostal margin to feel for spleen. As you reach the left subcostal margin, ask the patient to turn slightly towards you (his right side) , and palpate in the left subcostal area.
5. Kidney
Place one hand under the patient in the right flank region and the other hand on top and try to ballot the kidney between the two hands. Repeat for the left side.
How to differentiate between liver, spleen and kidney
| Liver | Spleen | Kidney |
| Dull | Dull | Resonant |
| Moves with respiration | Moves with respiration | Does not move with respiration |
| Notch | Ballotable | |
| Cannot get above it | Cannot get above it | Can get above it |
| Right hypochondrium | Left hypochondrium |
- Percussion
- Shifting Dullness (if distended)
- Fluid thrill
- Auscultation
- Bowel sounds
- Liver bruit
- Renal bruit (hypertension, neurofibromatosis)
- Other (Mention that ‘ I would also like to examine the patient’s….)
- Hernia orifices
- External genitalia
- Back and perianal area
- Inspect stool
For renal examination:
- BP
- Urinalysis
- Assess for signs of steroid toxicity
GI Revision Notes
Portal hypertension consists of:
- Splenomegaly
- Ascites
- Portosystemic shunts (Caput medusae, haemorrhoids, oesophageal varices)
Causes of portal hypertension:
- Prehepatic-Portal vein thrombosis (thrombophilia), postnatal umbilical vessel catheterization, sepsis
- Hepatic – cirrhosis, congenital hepatic fibrosis
- Posthepatic – Budd-Chiari syndrome, (hepatic vein obstruction), heart failure
Causes of hepatomegaly
1. Structural: Extahepatic biliary atresia, choledochal cyst, intrahepatic biliary hypoplasia, congenital hepatic fibrosis, polycystic disease
2 . Storage/ metabolic:
– Carbohydrate- glycogen storage disease (Type 1,3,4,6), hereditary fructose intolerance, galactosaemia,, mucopolysaccaridoses-
– Mineral: Wilson’s disease, juvenile haemachromatoses
-Nutrition: Protein calorie malnutrition, TPN-Bile flow: progressive familial intrahepatic cholestaisis syndrome
-Protease: Alpha-1-antitripsin
-Electrolyte: CF
– Amino acid: Tyrosinaemia type 1, urea cycle disorder
-Lipid – Gaucher, Nieman-Pick diease, cholesteryl ester storage disease
3. Haematological: Thalassaemia, sickle cell disease, ALL, AML CML
4. Heart/ Vascular: Conestive heart failure, constrictive pericarditis, obstructive IVC, Budd-Chiari syndrome
5. Infection: Viral – rubella, CMV, coxsackie virus, echovirus, hepatitis ABCDE, EBV ; Bacteria – E.coli TI, TB, syphilis ; Parasite – Malaria, toxoplasmosis, Schistosomiasis
Causes of splenomegaly
- Haematological causes
- Lymphomas
- Leukaemia
- Myeloproliferative disorder (myelofibrosis, CML)
- Haemolytic anaemia (Hereditary spherocytosis, sickle cell anaemia, G6PD, thalassaemia)
- Extramedullary haemopoiesis (Thalassaemia)
- Infections
- Acute: Endocarditis, typhoid
- Chronic: TB, brucellosis
- Parasite: Malaria, schistosomiasis, Kala azar, toxoplasmosis
- Inflammation
- Rheumatoid Arthritis (Felty’s syndrome)
- SLE
- Sarcoidosis
- Idiopathic Thrombocytopenic purpura
- Other
- Portal hypertension
- Amyloidosis
- Gaucher’s disease, Nieman Pick’s disease
- Tropical splenomegaly
Causes of hepatosplenomegaly
- Hepatic: Cirrhosis, congenital hepatic fibrosis, biliary atresia, sclerosing cholangitis
- Haematological: Thalassaemia, hereditary spherocytosis, sickle cell anaemia
- Infection: EBV, TORCH
- Malignancy: Leukaemia, lymphoma
- Metabolic: alpha1-antitripsin, tyrosinaemia, cystic fibrosis
- Storage disease: Gaucher (long term), Niemann-Pick disease, mucopolsaccharidoses
Causes of ascites
- Cirrhosis
- Congestive heart failure
- Hypoalbuminaemic states (nephrotic syndrome, malnutrition)
- Infection: TB
- Malignancy
- Hepatic vein thrombosis
- Meigs syndrome
- Pancreatitis
Indications of liver transplant
- Acute liver failure
- Decompensated chronic liver disease
- Liver-based metabolic disease
- Liver tumour
Pictures of ACE/ Stoma/ PD/ PEG / PEJ/ mitrofanoff
Author: Dr. Katherine Fawbert and Dr. Huey Miin Lee


very good notes and useful for me
When I initially left a comment I seem to have clicked the -Notify me
when new comments are added- checkbox and from now on every time a comment is added I get 4 emails with the exact same comment.
Is there an easy method you can remove me from that service?
Kudos!
Yes it’s a good revision site – but working in HE with advanced paediatric NP’s it’s also a great learning and teaching resource – thank you!
very very informative site
thanks, very useful for the clinical exam preparation
Thanks, well done
very nicely prepared and very systamatic